Soap Notes Medical Chart Printable – (source) to illustrate how a soap note works, let’s roleplay. The soap note and medical chart may seem pretty straightforward and conventional. Soap notes, once written, are most commonly found in a patient’s chart or electronic medical records. Please be mindful of these and use sparingly.
Icu Soap Note Template Pdf Template
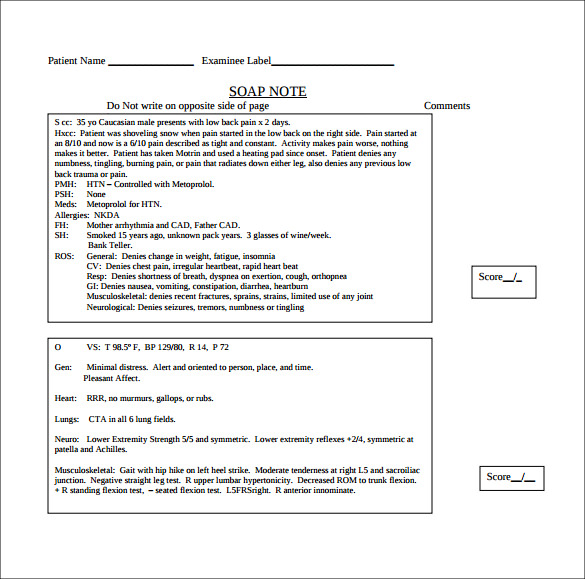
Soap Notes Medical Chart Printable
For example, si for suicidal ideation is a common A common method of documentation employed by many healthcare providers is using the soap note, which is an acronym for subjective, objective, assessment, and plan. The templates are available in pdf format and the file size starts from 15kb.
Subjective, Objective, Assessment And Plan.
Alter or add to original chart notes once they have been documented. Specify brand name, lot number and conditions whenever possible. Here’s how to write soap notes.
Printable Soap Notes Soap Notes This Simple Soap Note Page Is Perfect For Medical Professionals, With Divided Subjective, Objective, Assessment, And Plan Sections.
The soap note is a way for healthcare workers to document in a structured and organized way. If the diagnosis is already known and the findings of your assessment remain in keeping with that diagnosis, you can comment on whether the patient is clinically improving or deteriorating: Get the most out of soap notes templates.
Using A Template Such As Soap Note Means That You Can Capture, Store And Interpret.
Soap notes are a helpful method of documentation designed to assist medical professionals in streamlining their client notes. Learning how to write a soap note can be one of the most effective ways for clinicians to track, assess, diagnose, and treat clients. How does a soap note work?
Here Are Some Steps And Tips To Write Effective Soap Notes;
One way to make notes in a patient's dental record uses the acronym soap: Then, provide all the information in the subjective. Besides cutting down on waste, migrating to a digital version of soap notes provides a variety of benefits including:
Smartly Designed, Templates For Your Discharge Summary, Clinical Notes, And Consultation Notes;
This system can minimize the risk of failing to include important details in the record. Download free version (pdf format) The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers.
Click Here To Get The Soap Note Template!
How to write soap note template? This site offers over 30 free soap notes templates for medical specialties including psychiatry, asthma, psoriasis, pediatric, and orthopedic. This might include subjective information from a patient’s guardian or someone else involved in their care.
New Fully Customizable Soap Notes.
Administrative processes can be simplified At first, download the editable and printable soap note template from any site. The soap note format helps medical professionals to record patient data easily through a highly structured style.
To See What A Soap Note Template Looks Like, Check Out (And Use!) This Example From Process Street:
Here’s how to write soap notes. This highly structured style often enables workers to easily find patient records and, when needed, retrieve key information Information about the patient and the doctor can be recorded at the top, as well as the diagnosis and procedures.
Where A Client’s Subjective Experiences, Feelings, Or Perspectives Are Recorded.
You Can… Add Past Medical History And Past Visit Notes Directly Into Your Soap Note;
Document your impression of the diagnosis (or differential diagnosis): Include symptom dimensions, chronological narrative of patient’s complains, information obtained from other sources (always identify source if not the patient). Soap is an acronym for the 4 sections, or headings, that each progress note contains:
However, Some Very Useful Functionality Can Make Your Charting Experience Much Faster.
Add a previous diagnosis from the assessment section Let us review the four components of a soap note: A handful of commonly used abbreviations are included in the short note.
Choose From 15 Different Question Types Including Short Answer, Multiple Choice, Pain.
Download soap note templates for easy and paperless documentation of patient data. Both meet minimum documentation standards and are acceptable for use.

Massage therapy, Soap note, Medical printables

SOAP Notes Dentistry Pages format

Medical Soap Note Template Medical Progress Note Template Pdf LZK

Image result for sample soap note chart
Icu Soap Note Template PDF Template

40 Fantastic SOAP Note Examples & Templates Template Lab

023 Soap Note Example Mental Health Ems Format Template inside Soap

10+ Soap Note Template Free Download Word, Excel, PDF Format!!

Medical Chart and SOAP Notes Templates Practice Fusion

Image result for surgical notes sample Soap note, Notes template

5 Best Printable Chiropractic Forms Soap Note

What are SOAP Notes in Counseling? (+ Examples)

Nanda Nursing 19+ Nursing Patient Organization Sheets
9+ Medical Note Templates Free Sample, Example, Format Download

Chiropractic Soap Note Template Free Addictionary